The Strange History of Medicinal Cannabis in Australia
A Tragi-Comedy in Two Acts & Three Phases
In early 2016 media both domestic and global reported that Australia had ‘legalised medical marijuana‘.
What they were referring to was passage of the Narcotic Drugs Amendment Bill in the Australian Parliament, achieved in almost record time and with cross-party support, on 24th February that year.
Such headlines though weren’t the entire story and nor did they predict what would follow: three years of bitter, often desperate struggle on the part of patients who felt they’d been badly deceived and a government many believe acted only for show. Claims to have made cannabis available seemed empty, they all felt, while every effort was made to ensure it stayed as far beyond the reach of those needing it as ever it was before legislative changes occurred.
Some background
For a start, the Bill didn’t ‘legalise the use’ of medical cannabis or cannabis medicines at all; prescribing had always been technically (if not practically) possible using the Federally-run ‘Special Access Schemes’ which, in certain circumstances, allow doctors to obtain drugs or therapies not registered (or generally allowed) for use in Australia. On top of these, one such medicine – Sativex – had already been formally approved by Government’s medical regulator.
What the Narcotic Drugs Amendment Bill did do though was modify the existing Federal Narcotic Drugs Act of 1967 so as to permit, at Commonwealth level, the lawful cultivation of cannabis and manufacture of cannabis products for medicinal and research purposes for the first time in more than a half-century.
It had been a long time in coming. For decades, as elsewhere, Australia had been hotly debating the matter; some argued for an end to cannabis prohibition altogether, others for its medical use while others still wished it to remain completely forbidden. As far back as 1994 a background paper prepared for for the New South Wales Government noted:
‘A number of prominent Australians, including politicians from all major parties, were signatories to a charter calling for the decriminalisation of cannabis. Although such resurgence of interest in the issues surrounding the cannabis debate has occurred in the past with no resulting change to legislation, the current level of interest in the topic across all levels of Australian society suggests that cannabis is an issue that has yet to be resolved to the satisfaction of all concerned.’
By the end of the noughties though, a growing body of evidence, mainly from overseas, was suggesting real therapeutic benefits were to be had – if not from the plant itself then at least some of the chemicals within it. Indeed, a small number of ‘cannabinoid-based medicines’ – both synthetic and organically derived – were registered in the US and Great Britain, and, as we’ve noted, one of them, Sativex – though not marketed until 2018 – was registered for use in Australia.
Cultivation of industrial hemp, once an Australian main-stay, had, from the late 1990s also been gradually re-introduced (though notably not as a foodstuff – that too would take until 2018) and by 2013, where cannabis generally was concerned, matters were reaching a head.
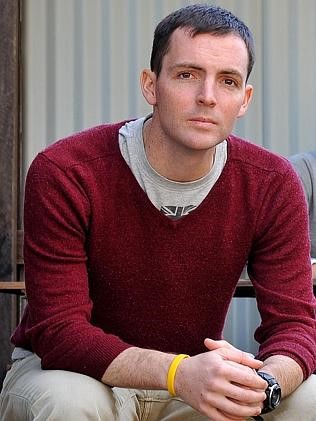
This was in large part due to the work of one woman: New South Wales mother and former nurse Lucy Haslam.
Her son Dan, who sadly died in early 2015 at just 25, had Stage 4 bowel cancer and suffered horrifically from the effects of his chemotherapy.
Cannabis, it turned out, was the only thing that provided relief and, feeling aggrieved at finding themselves criminalised for using the one treatment that proved effective, Lucy and Dan began campaigning for a change in the law.
Things gathered momentum; quickly gaining support locally, first from the town newspaper then the police and the Mayor, eventually they pulled on board then-NSW premier Mike Baird. A year later the Premier, by this time a family friend, wrote a Daily Telegraph article ‘How a young man changed my mind on cannabis’.
His government had, just two years earlier, ignored a Parliamentary Committee Report which spoke of the drug’s potential and recommended legislation be relaxed, so Baird’s involvement marked a turning point in what had become an historic if complex journey.
Australia, with it’s eight States and Territories, is, like America, a legislative and regulatory patchwork albeit very consistent where medicines and their Scheduling are concerned. The Therapeutic Goods Administration (equivalent to the FDA in the US) governs the approval, registration and categorization of all drugs nationally, placing them within two important registers – SUSMP – the Standard Uniform Scheduling of Medicines and Poisons (known as the ‘Poison Standard’) and the ARTG – the Australian Register of Therapeutic Goods which lists drugs approved for domestic use. States then take their cue from SUSMP and adopt the same Schedules and Appendices.
Unlike the US however, cannabis was, in 2014, completely forbidden in all States and Territories, being a Schedule 9 substance within the Poison Standard. Although treated with varying degrees of seriousness by respective jurisdictions (Queensland for example places it alongside heroin, ice and cocaine where sentencing guidelines are concerned while in the Australian Capital Territory possession of small amounts has in practice been decriminalised) still, there was no recognition anywhere that cannabis might be anything other than a ‘Prohibited Substance’.
The impact of the Haslams’ campaign therefore cannot be over-stated.
The interest and media it garnered nationally – which by mid-2014 embraced press, radio and TV and now included the stories of dozens of similarly-off families who’d come forward after hearing of Dan’s situation – led to a flurry of political activity.
The Capital Territory and States of Queensland and Victoria launched their own Public Inquiries (here and here – ACT unavailable) as did Tasmania, which happens to provide half the world’s licit opium poppy straw and which was the prospective location for an imagined new cannabis industry.
So positive was the mood at the time, at short notice and rather like the proverbial bumblebee unaware of its supposed aviatorial inability, Lucy decided to run a Symposium, the first of its kind in the country. Thus, at the behest of a determined housewife and mother from a small town in provincial Australia gathered some of the legends of the cannabis panoply – Ethan Russo, Lester Grinspoon, and film-maker Zack Klein naming a few. Politicians taking part included Mike Baird and Federal Greens’ Leader Senator Richard di Natale, whose efforts later that year would make history.
It was here at the Symposium, behind the scenes and during informal networking sessions, the seeds of a future domestic cannabis industry can truly said to have been planted, as well as the initial idea for what would later become the ‘Lambert Initiative for Cannabinoid Therapeutics’ at Sydney University. This 10 year-long, generously funded project, one of the biggest and most richly endowed centres of its type in the world, was the brain-child of two Sydney academics presenting at the event and Michael Lambert, another speaker, whose daughter Katelyn suffered with intractable seizures. Michael’s father Barry was a Rich Lister businessman so the meeting was a fortuitous one – an unprecedented $34 million bequest was to follow.
Some months later, at national level – and crucially – the Australian Greens along with other cross-bench MPs tabled a Bill in the Senate: the Regulator of Medicinal Cannabis Bill 2014. It recognised what most other countries with existing MC systems had long realised: that to make such medicine genuinely available, for a plethora of reasons, processes designed to regulate single molecule pharmaceutical products synthesised or refined in a laboratory are completely unsuited to cannabis. Thus Governments as diverse as Canada, Israel, Germany and The Netherlands have either established entirely new stand-alone regulators or created a specialist division within their existing regimes. An paper by Israeli researchers in the September 2018 edition of Nature articulates the logic behind this extremely effectively – a vastly important aspect of cannabinology the medical establishment in Australia was and still is determined not to acknowledge:
‘Most clinical studies of Cannabis today focus on the contents of two phytocannabinoids: (-)-Δ9-trans-tetrahydrocannabinol (Δ9-THC) and cannabidiol (CBD) regardless of the fact that the plant contains over 100 additional phytocannabinoids whose therapeutic effects and interplay have not yet been fully elucidated.
‘This narrow view of a complex Cannabis plant is insufficient to comprehend the medicinal and pharmacological effects of the whole plant.’
To it can be added the fact that, as cannabis clinicians know only too well, the drug’s effects often vary markedly between individuals while different strains often possess quite different properties. It means of course that treatment regimes demand high levels of personalisation and to go with them significant trial and error. And it also means for that reason the drug does not lend itself particularly well to clinical study by conventional methods: simply, Double-blind, Randomised, Controlled Trials are inadequate because, where cannabis is concerned, what suits one individual may very well not suit another.
This was precisely what the Greens’ and cross-bench Bill understood, and it sailed through the Upper House unopposed.
Putting it bluntly, at that stage the Government had been caught with its pants down. A poll conducted by the Seven TV channel received not far shy of 3 million votes, 97% of which were in favour of cannabis for medical use. It was borne out not long after by research done by Roy Morgan, one of Australia’s top consumer, industry and market research outfits. Alongside, a petition of around 250,000 names presented irrefutable proof of overwhelming public support; something unquestionably had to be done.
Another Public Inquiry ensued, this one at Federal level, which set out to examine the ‘Regulator’ Bill in fine detail. It comprised hundreds of Public Submissions, three days’ worth of Public Hearings and ran through 2015.
In the February of that year Dan tragically passed away. He died believing (correctly) that he and his mother had accomplished much together and convinced (not quite so correctly) matters would continue along that same trajectory. Lucy promised she’d continue the fight and gave evidence to the Inquiry a month later.
Dan’s Law was put in place to legalise the cultivation of medicinal cannabis in Australia. But was it all for nothing?

Expert Opinion
In September 2018 the Huffington Post ran an article, not about cannabis but on fat-shaming.
Titled ‘Everything You Know About Obesity Is Wrong‘, author Michael Hobbes (himself referring initially to scurvy rather than weight) noted, insightfully:
Every discovery in public health, no matter how significant, must compete with the traditions, assumptions and financial incentives of the society implementing it.‘
Many have needlessly died, Hobbes says, as a result of this ‘failure to implement’ – arguing many more will die because of the ‘counter-productive ways we addressed the obesity epidemic.’
The same principle, many of us claim, holds true with cannabis.
Of the more than 300 Submissions received during the Public Inquiry, the overwhelming majority, including from experts – and more importantly the relatively few experts in Australia with an in-depth knowledge of cannabinology – were fiercely in favour of Richard di Natale’s Bill.
Those ranged against it were telling, since they comprise exactly the same voices that to this day stand in vehement opposition to the reintroduction of cannabis to the physicians’ armementarium.
Their arguments – that the drug is ‘dangerous’, ‘untested’ and that a ‘lack of evidence’ exists for its efficacy – now sound increasingly shrill, desperate and hollow in light of the data that pours in almost hourly. Yet such positions are, in 2018, largely unchanged from four years back.
Peak bodies such as PainAustralia and Palliative Care Australia, both openly and handsomely funded by big opioid manufacturers such as MundiPharma who make OxyContin came out strongly against the Regulator Bill, as did the Australian Medical Association as well as the specialist medical colleges. In particular the anaesthetists’ and pain specialists’ body ANZCA / Faculty of Pain Medicine (FPM), another significant beneficiary of Big Pharma largesse, has pushed back violently against the drug at every available turn. (A look at its National Pain Strategy (Appendix 4: Grants p 73) is revealing).
Despite all reasoned arguments to the contrary, including those from within the 2017 National Academy for Science, Engineering and Medicine Review which famously found ‘…conclusive or substantial evidence that cannabis or cannabinoids are effective …for the treatment of chronic pain in adults,‘ ANZCA remains adamantine in its opposition, widely publicising its view in June 2017 that:
‘The gap between the current evidence and community (and political) perception of benefit is now big enough to demand a ‘harm minimization’ approach that will allow Fellows on the clinical frontline to manage these expectations as well as pursue potential clinical research.’
Indeed, as late as September this year, Michael Vagg, FPM’s Acting Dean, told the Cairns Post that ‘access to good quality, co-ordinated pain medication is a better option than medicinal cannabis‘ because THC – which he acknowledges is necessary for any analgesic effect – would result in users being ‘sent mad’. His organisation crowed at the coverage and added on its own website that:
‘The print story was syndicated to nine other News Limited online sites including the Herald Sun, The Daily Telegraph, the Geelong Advertiser and the Courier-Mail reaching a readership of 100,000 people.’
The Faculty’s current position on the matter meanwhile (as of 2018) remains that:
‘At the present time, the scientific evidence for the efficacy of cannabinoids in the management of people with chronic non-cancer pain is insufficient to justify endorsement of their clinical use.’
During the 2015 Inquiry, these organisations, together with the Federal Department of Health and Medicines Australia – the powerful lobby group representing the country’s pharmaceutical industry – unflinchingly insisted, and against other, highly expert advice – that cannabis be treated ‘like all other drugs’.
Medicine Australia’s view of the matter in fact summarises the position quite well – ‘(we do) not see a need for, and therefore (do) not support, the introduction of the Regulator of Medicinal Cannabis Bill 2014 to establish a Regulator of Medicinal Cannabis and a system of regulating medicinal cannabis that is entirely separate from the TGA,’ the group said, adding ‘Pharmaceutical manufacturers of prescription medicines are subject to a strict regulatory regime to ensure medicines made available to the Australian public are safe, effective and of a high quality,’ with the inference that herbal cannabis did not and could not meet such criteria.
So concerted, and so consistently ‘on message’ are these outspoken critics of cannabis and so successful have they been at halting real progress in the area, it’s easy to concur with Kent University’s Alex Stevens of the UK Advisory Council on the Misuse of Drugs when he writes about policy-making:
‘Actors who share interests and norms come together in policy constellations. Strategic action within and between constellations creates policies that may not take the form that was intended by any individual actor. These policies do not result from purely rational deliberation, but are produced through ‘systematically distorted communication’. They enable the most structurally favoured actors to institutionalise their own normative preferences and structural positions.’
Nevertheless, the Senate’s Legal and Constitutional Affairs Legislation Committee which considered the evidence recommended in its final report that the Greens Bill be enacted.
Clearly panicked and with a General Election on the horizon, the Government responded with an alternative – the Narcotic Drugs Amendment Bill previously mentioned – which baulked at the creation of this separate regulator. Instead – and remember this was against what the Committee suggested – the Bill would place cannabis not in the hands of a stand-alone body but in those of the its existing organisation the Therapeutic Goods Administration. To add insult to injury, it was rushed through both Houses with unprecedented haste on 24th February 2016 – the anniversary of Dan Haslam’s death – and cynically christened ‘Dan’s Law’.
At this time the drug was also being re-scheduled: 98% pure CBD products (by ‘co-incidence’ the same as that of Epidiolex created by GW Pharmaceuticals the firm behind Sativex) were placed into Schedule 4 of the SUSMP – available by prescription only. Medicines containing THC found their way to Schedule 8 which are ‘Controlled Drugs’ such as opioids and thus subject to State approval. Black market cannabis remained within Schedule 9, a ‘Prohibited Substance’ – so now, spread across multiple Schedules, cannabis was in quite a mess.
And unfortunately, the rest is (a pretty disastrous) history.

United in Compassion have continually sought support from politicians and medical practitioners to give patients access to medicinal cannabis
Three Phases
In hindsight, Australia’s dalliance with this medicine (for in reality it’s been no more than that) can be said to have fallen broadly into three phases. First came the massive campaign for its legalisation staring in early 2014, the culmination of which, was passage of the grossly sub-standard Narcotic Drugs Amendment Act 2016 – a deliberately imperfect substitute for the original Regulator Bill introduced to do little else than ensure TGA control and keep Australia compliant with the various UN Drug Treaties.
Next – throughout most of that year and the following – came the creation and implementation of a morass of Federal and State regulation and legislation that would govern how the medicine was (or more accurately wasn’t) produced. It would also dictate, more or less, for what and by whom it might be administered – as well as the means by which patients could, in theory, get hold of it.
As Rhys Cohen of the Lambert Initiative put it in late 2018, the system was ‘bloated with committees, expert advisory boards and bureaucracy. It seemed almost guaranteed to ensure that access would not occur, with a whole raft of onerous requirements at both State and Federal government levels’ which in practice meant doctors having to make detailed applications to the Federal Department of Health and often to the State Health Department on top. In most cases the endorsement of a medical specialist was also required, if they weren’t indeed specialists themselves.
Such applications would need to specify the clinical history of the patient; demonstrate all other available therapies were exhausted; explain the medical and scientific literature they’d researched to support their decision to try cannabis and then to specify and justify the exact product plus the dosage and treatment regime.
And quite earnest efforts by the Federal Health Minister of thee time to ‘streamline’ the mechanism with a single application process to cover both TGA and State applications has proven itself a damp squib, with a patchwork of approval rates across States, so matters were not much improved.
It was during that ‘second phase’ though an ‘Expert Advisory Council‘ was formed, supposedly to offer input into policy-making around the area but comprising some of the most virulent and noteworthy opponents of cannabis anywhere to be found Australia, at least one of them with a reputation extending well beyond the country’s own shores. Meanwhile none of the internationally renowned scientists and academics at work in the space locally (and there are a few) were invited to sit on the thing – which speaks volumes about why the Council was in fact convened. This ‘chapter’ arguably ended in December 2017 when the Federal Government published a sort of ‘last word’ in its project to ‘regulate’ the drug – a series of ill-received ‘Clinical Guidances‘.
Supposedly created to inform doctors and others on the practical use of the medicine, the documents were based on highly selective literature reviews – historical RCTs of cannabis products in respect of a limited number of indications.
As one might imagine, given eighty-odd years of the drug’s prohibition – effectively throttling research into anything other than its presumed harms – relatively few such studies were found to by the TGA reviewers to exist; access to materials and funding to explore any benefits had for decades been all but impossible to procure.
Unsurprisingly then, they concluded ‘little evidence existed’ in terms of efficacy but caused outrage among advocates by precluding anything other than English language Randomised Controlled Trials and making no reference to the increasingly wide clinical practice of cannabis medicine globally nor the expansion of ‘demographic and prescribing data’ currently emerging in light of it.
They also contained little or nothing in the way of information that might genuinely help guide prescribing – but possibly most indicative of all they were produced long after the TGA and others had been given an early English translation of the ‘Green Book’ – an Israeli Ministry of Health-produced manual arguably the most practical prescribing guide in the world. That publication was literally placed in the hands of a TGA official by a member of an Israeli delegation during a visit to Australia in 2016 which meant the Government had the tome in its possession well before its own volumes were compiled. Thus do the Australian documents – to which doctors are officially being urged to turn if considering the prescribing of cannabis – in reality serve to inhibit rather than to encourage the medicine’s use.
The Israelis were very explicit too, when they came to Australia bearing gifts. ‘We don’t know everything about this plant,’ members of the delegation said, ‘but we do know more than anyone else. It is too safe not to use and we feel it’s immoral to prevent access to something that obviously works so well.’
Associate Professor David Caldicott of the Australian National University who teaches the most thoroughgoing of the three RACGP-accredited ‘Medical Cannabis Courses’ available in the country was forthright. The week the ‘Guidances’ were published he publicly weighed in on Twitter, noting – without concern for diplomacy – that:
‘In just a decade’s time, they (the Guidances) will be mocked as an example of the abuse of science. (They are) political, designed to arrive at conclusions that suit parties other than patients. The sad reality is these documents …will do next to nothing to change the status quo – an illicit market of uncertain provenance, accessed by desperate people. They don’t tally with the experience of tens of thousands in Australia – millions worldwide – and so will simply be ignored, even by doctors who choose to educate themselves, overseas and online, about the ‘actual’ pros & cons of medicinal cannabis.’
These are issues though encountered not just in Australia but seemingly wherever and whenever the conservative (often dominant) elements within the healthcare professions choose to engage on the issue: the problem of ‘evidence’ seems, for now, an intractable one.
As Caldicott and others have identified – and as one patient eloquently expressed it on Twitter –
‘It’s so frustrating to see marijuana prohibitionists debating IF cannabis is efficacious in treating pain when patients are screaming at the top of their lungs “YES, YES IT IS!” For them to just blatantly ignore the very people who are suffering is more than wrong. It’s evil.‘
But for sceptics and opponents, very conveniently one could argue, the only acceptable data is that represented by RCTs– the so-called ‘Gold Standard’ of ‘Evidence Based Medicine’.
Never mind that, as we’ve already suggested, cannabis is largely unsuited to such a rigid approach; never mind that millions of people worldwide are finding relief while providing vast lived experience that amounts to overwhelming ‘demographic’ (or ‘Real World’) data’ as Caldicott and others refer to it. And never mind the growing pockets of genuine (and readily accessible) expertise in prescribing such medicine within jurisdictions that already permit it. No amount of reasoning, no argument, no stack of peer reviewed papers has been large enough shake these organisations and individuals from their intransigent avowal that only RCT’s can pass muster.
Challenging this ingrained belief though is not without intellectual or clinical legitimacy; no less a figure than Louis Lasagna – a giant within the pantheon of clinical pharmacology and author of the revised Hippocratic Oath – said of such trials:
‘In the last 40 years there has been a radical change in the ways of obtaining information about therapeutic agents that are considered valid by the scientific establishment and by national regulatory authorities. We have witnessed the ascendancy of the randomized, double-blind, controlled clinical trial (RCCT), to the point where many in positions of authority now believe that data obtained via this technique should constitute the only basis for registering a drug, or indeed for coming to any conclusions about its efficacy at any time in the drug’s career. My thesis is that this viewpoint is untenable, needlessly rigid, unrealistic, and at times unethical.’
That’s a big (some would say controversial) thesis, but one that makes absolute sense in the cannabis realm, for reasons already discussed.
In response, many see N=1 trials as a plausible solution to Australia’s impasse in relation to this.
Justin Sinclair, a research fellow and pharma-cognosist at NICM Health Research Institute at Western Sydney university and one of Australia’s most knowledgeable educators in the sphere of cannabinology, outlined such thoughts to the TGA in an open letter to the regulator last year.
‘According to the National Health and Medical Research Council (NHMRC), evidence comes in (various forms),‘ Sinclair pointed out, and ‘This ‘hierarchy of evidence’ underpins the clinical decision-making process of government departments, research institutes and universities as well as individual medical practitioners making informed clinical judgements.’
And N=1 one trials, he noted, very much fell within such a hierarchy.
‘This level of evidence considers an individual patient as the sole unit of observation in a study investigating efficacy or side-effect profiles of different interventions, with the goal being to determine the optimal intervention for an individual patient using objective data driven criteria and outcome measures’.
As such they could be used to gather evidence about cannabis and allow patient access – a view with which David Caldicott and many others, including Lucy Haslam concur.
Like all else of a pro-cannabis, pro-patient bent however, the highly detailed, well-referenced letter fell on completely deaf ears; Sinclair received no response.

Dr David Caldicott is a founding member of the Australian Medical Cannabis Observatory; the AMCO was created to establish the infrastructure and support systems that an industry will require.
Currently….
‘Phase three’ – the current one – of this convoluted and frustrating journey has left all concerned trying to make sense of the landscape and discern how best to move forward. And for many – especially patients – the situation is far from a happy one.
Numbers have not yet been been discussed. At time of writing (March 2019) out of (at least) 100,000 people reckoned to be using the drug solely for medical purposes in Australia only around a couple of thousand or so are using a legal, prescribed product outside of clinical trials and/or ‘compassionate access’ schemes. To put that in context, Germany, to take just one example, now has well over 50,000 authorised users from next to zero in 2017 – a year after the law was changed in Australia.
But here clinical trials and other ‘research’ seem to be where everything is at at the moment – though in many instances such exercises appear more like re-inventing the wheel or covering ground already well-tilled, as if Australians are somehow physiologically divergent from all other humans elsewhere . As NASEM has demonstrated, we know cannabis works for some types of pain, we know it works for chemotherapy-induced nausea and vomiting. Yet here we are running trials for those very conditions in Australia while simultaneously trialling synthetics; one company in particular claims its artificial CBD is superior to the natural molecule because of ‘the potential degradation of CBD by gastric acid into THC’ – a myth that has been largely debunked. In Queensland though this compound is one of only three cannabis-related products (all CBD) the State’s Health Department and neurologists working within it will even consider prescribing for childhood refractory epilepsy.
A $ multi-million, Federally funded ‘Centre for Cannabinoid Clinical and Research Excellence’ has also been initiated, its main accomplishments thus far having been to attempt to alter the conversation from any discussion of ‘medicinal cannabis’ to that of ‘medicinal cannabinoids’ since according to the pervading philosophy the herbal or whole plant variant has no place in medicine at all.
‘Currently the majority of US Sates have one of the various legislative regimes to access medicinal cannabis for a range of conditions despite the inconclusive evidence base for safety and efficacy of cannabinoids for the majority of those conditions,‘ the Centre chirpily asserts in one of its (yet to be published) papers.
Elsewhere, particularly in New South Wales, other trials have been established primarily to prevent wider access, according to Lucy Haslam.
Speaking in 2017 she claimed that Mike Baird, as NSW Premier, was deliberately thwarted in his efforts to help people by then Health Minister Jillian Skinner abetted by various officials. ‘How can we stop this?’ Skinner apparently asked, to be told: ‘Just tie it all up in clinical trials and base access on the outcome of those.’ And for over two years that is exactly what happened, though in recent months and to the horror of bureaucrats, the State has taken a few minor steps to relax things.
In the midst of these rather gloomy circumstances however are to be found a few glimmers, if not of optimism, then the hope that something positive will eventually emerge from what has been mostly a train wreck.
While some of the trials were historically created to be dilatory and as a means of keeping this much-needed medicine as far away from patients as possible, others, current or forthcoming, show promise. For example RCTs of medicinal cannabis in adults with Tourette’s Syndrome and a Phase 2 trial assessing the tolerability of two different ratios of the drug in patients with Glioblastoma multiforme (GBM) look genuinely ground-breaking and in areas little researched.
In total, according to the TGA’s Office of Drug Control, something over thirty such exercises (of varying size and significance) and are currently underway in Australia which it expects will ‘contribute positively to the amount and quality of evidence to either support or contradict the use of medicinal cannabis as an approved treatment across a range of health conditions and symptoms,’ the word ‘contradict’ saying much of officialdom’s view.
Beside these is a growing canon of work from the Lambert Initiative which thus far has managed to produce major papers on, respectively, attitudes of Australian GPs towards use of the medicine, composition and use of ‘artisanal’ (i.e. illicit) products for childhood epilepsy in the community and a survey of the drug’s use among people with epilepsy – which discovered nine out of ten patients who used cannabis found it more efficacious than other therapies. Whilst badly misreported by elements within the media, a further survey, ‘Medicinal cannabis in Australia, 2016‘ discovered the most frequent reasons for its use among adults were were anxiety, back pain, depression and sleep problems.
Future and current undertakings include the soon-to-be-published results of a cannabis and driving impairment study, a youth anxiety trial and several pilot collaborative clinical studies that should be up and running inside 12 months – among them research into cannabis and primary insomnia, alcohol detoxification, dementia, anorexia nervosa and PTSD.
Grabbing the headlines in October 2018 was also a ground-breaking survey from Justin Sinclair’s organisation, Western Sydney University’s NICM Health Research Institute, Australia’s peak body in integrative and complementary medicine research and policy.
An online survey, conducted in collaboration with of Endometriosis Australia and Endo Active, heard from 484 women about how they dealt with pain associated with endometriosis, of which 13% answered cannabis. Other techniques included heat (the most common) and exercise. However when asked to score the pain relief out of ten, cannabis came out a clear top at 7.6. Women using cannabis also reported reductions in pharmaceutical usage, with 56% of cannabis users in the survey reporting reductions in their endometriosis-related medication by more than 50%. The types of medications reduced were not specified.
As Dr Mike Armour, a post-doctoral research fellow at NICM remarked, ‘the data indicates women are using the drug regardless of its legality so its effectiveness needs to be explored‘. In fact further research has already been planned starting next year investigating how cannabis may assist women dealing with this incredibly painful condition.
It would take a book (and a lengthy one) to do justice to every twist and turn in this story, every high-profile arrest; the ‘medical refugees’ leaving Australia to source their medicines in more sympathetic regulatory climes, the deaths of a number of children; here we just scratch the surface.
And what of the ‘Licensed Producers’ to whom we have thus far have not even alluded?
Twenty or so are listed on the Australian Stock Exchange and 46 have Federal licences to grow and / or research and / or manufacture cannabis products and smaller handful with the additionally required State Permits to grow. Of these an estimated three (maybe four) have managed to get seeds in the ground and (again, at time of writing) only one has a product to market.
All this was far from Dan and Lucy Haslam’s vision when the groundswell of public opinion seemed to sweep them toward what looked like victory. Imported products – mainly Canadian oils – mean today any of that tiny number of patients fortunate enough to have found medics willing to do battle with a negative and overweening bureaucracy are paying in the region of $35,000 per annum (often more) for a medicine that by rights should cost a fraction.
The message here, if there is one, is that policy-making in this area has proven itself a microcosm of a far wider administrative malaise which has ended up costing the present Government dear. And barring a political miracle, Australian Labor look set to take power comfortably come the next General Election. The question remains though whether they’ll do any better – and currently it doesn’t bode well. In mid-October 2018 another debate took place in the Australian Senate – this one on a Bill that would have ended cannabis prohibition altogether (and which unsurprisingly fell on its second attempt).*
For the first time though since 2015 Labor gave an indication of where it stood in relation to the drug’s medical use when a Member said the following in the course of the deliberations:
With respect to medicinal use of cannabis, Labor policy is to work with the state and territory governments to ensure nationally consistent laws which allow lawful access to medicinal cannabis for those who are terminally ill or have other clinically identified medical conditions and where medical cannabis may benefit. If Labor wins government, we have committed that the Commonwealth government will become the national regulator of medicinal cannabis supplied to eligible patients and for research purposes. Labor has also committed to work with state and territory and federal regulators to improve controlled access to medicinal-grade cannabis for legitimate scientific and mental research work. Consistent with this role, under Labor the Commonwealth would establish rules—for licensing one or more producers of cannabis, for supply to medical patients and for research—subject to the best manufacturing practice and best agricultural practice to ensure safety, quality and security in the production and distribution process.
To the untrained eye – or even the trained one – it is impossible to discern how and where this differs an iota from the current (highly undesirable) system nor whether a change in Government will mean any improvement.
Certainly Lucy is trying with her #FixDansLaw campaign having’undeclared the victory’ of her Change.org petition.
From the above though, it is clear, advocates will have their work cut out to effect anything like the policy-change needed if the lot of patients needing cannabis products is to improve any time soon.
An election looks scheduled for May 2019. Watch this space for updates or the UIC Facebook page for updates.
* Updated June 2019. As most are aware, a ‘political miracle’ did occur at the aforementioned General Election (certainly PM Scott Morrison described it as such) with the Coalition winning a third term in office. Labor had, a week earlier, posted its new MC policy on the Change.org platform, largely confirming the misgivings of this article. The Greens meanwhile vowed to re-introduce the Regulator of Medicinal Cannabis Bill to the new Parliament.

Patients are the meat in the sandwich – often having to resort to the black market for medication.

Dan & Lucy Haslam campaigned for patient’s rights to medicinal cannabis. Lucy continues this fight following Dan’s death.


